Levels of Amputation
Introduction
When a limb has to be cut off (amputate) to treat a disease or an injury, the level at which the limb has to be removed is to be decided.
During the decision the following has to be considered :
the boundary of dead or diseased tissue
the extent of blood supply to the limb
suitablility of the remaining portion for a prosthesis (artificial limb)
present mobility and future mobility of the limb
cosmetic appearance
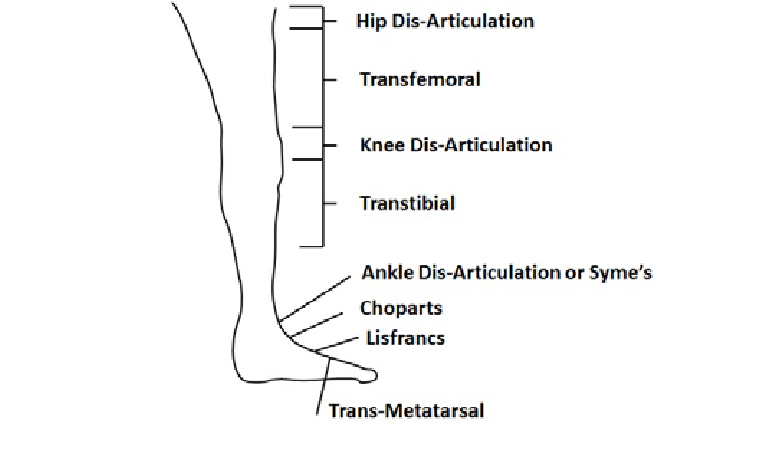
The various levels of amputation in the lower limb
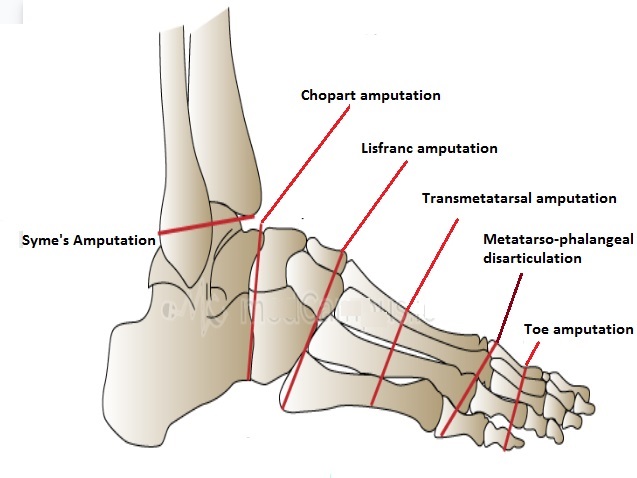
Toe amputation : disarticulation at one of the interphalangeal or metatarso phlangeal joints
Foot amputation : Transmetatarsal : partial foot amputation through metatarsals (usually due to wounds in the forefoot due to gangrene or infection
Midfoot and hindfoot amputations
Tarsometatarsal amputation (Lisfranc) - amputation of the forefoot at the trarsometatarsal line
Mid-tarsal amputation (Chopart) - amputation of the forefoot at the tarsometatarsal line.
Ankle disarticulation (Symes amputation) - amputation through the ankle joint.
These 3 types of amputations are mainly performed in children to preserve the length of the residual limb and to keep the epiphyseal plate intact.
Transtibial / Below Knee Amputation (BKA)
Amputation is done through the tibia and fibula, measurements are taken and flap lines marked out. Optimum length of residual bone is approximately 12-17cm;
The tibia should be beveled at approximately 45° to remove the sharp anterior edge, the fibula should ideally be approx. 1-2 cm shorter than the tibia. Long posterior muscular flap covering the distal end, attached ventrally to a shorter anterior flap
Knee Disarticulation Amputation (KDA) / Through Knee Amputation - Amputation done through the knee joint
Advantages
Long lever prevents contractures and allows consequently the movement control.
Maintains muscle length and strength
Preserves growth plates in children
Candidates for end bearing prosthesis
Conserve condyles and the patella
Proprioception and better distribution of pressure
Disadvantages
Bulky prosthesis
Poor cosmesis as knee mechanism is distal to the knee joint
More demanding surgical procedure with the risk of increased wound complications
Transfemoral / Above Knee Amputation
Amputation is done through the femur, measurements are taken and flap lines marked out.
The optimum length of the residual bone is approximately 7.5-10cm proximal to the superior border of the patella. Very short trans-femoral stumps often end up in abduction because there is an imbalance between the adductor and abductor muscles.
With a transfemoral amputation, the distal attachments of the thigh muscles are lost, in order to preserve their function and length, a myodesis may be performed to anchor the adductor (and sometimes hamstring) muscles to bone. The hamstrings and quadriceps may then be sutured together over the distal end of the femur – a technique called a myoplasty. It is a myoplasty of the antagonist muscles to help pad the end of the stump to perform Gottchaltk myodesis (adductor magnus trans-osseously fixed and covering the distal femoral end)
Advantages and Disadvantages For Long stump
Advantages :-
best lever
better muscular balance while preserving the strength of the adductors
energy efficient
candidate for ischial tuberosity bearing prosthesis
Disadvanges :-
reduced strength of the adductors
increased flexion and abduction
increased energy expenditure
Short stump
weak adductor muscles, causing a severe imbalance
the position of the stump often ends up in flexion and abduction
causes massive energy expenditure (effort) and the prosthesis can be heavy
Very short trans-femoral stumps often end up in abduction because there is an imbalance between the adductor and abductor muscles.
Hip disarticulation is amputation of the whole lower limb through the hip joint. A traditional hip disarticulation is done by separating the ball from the socket of the hip joint, while a modified version retains a small portion of the proximal (upper) femur to improve the contours of the hip disarticulation for sitting. A hip disarticulation results most often from trauma, tumors and severe infections, such as necrotizing fasciitis. Less often, it results from vascular disease and complications of diabetes. Many are wheelchair users but can be considered for ischial tuberosity bearing prosthesis. The risks for wound complications and mortality with this type of amputation is very high.
Hemi-pelvectomy (Hindquarter)
Amputation of the whole lower limb and ipsilateral hemi-pelvis[13] This type of amputation is most rare. They are likely to be a wheelchair user, some are considered for a trunk and contralateral ischial tuberosity weight-bearing prosthesis
Levels of upper limb amputations:
Fingers
Partial hand
Wrist disarticulation
Transradial
Elbow disarticulation
Transhumeral
Shoulder disarticulation
Scapulo-thoracic dissociation (forequarter)
There is a range of different prosthetics available for the upper limb; these range from hooks to passive orthotics that might mainly serve an aesthetic purpose to fully mechanical and functional limbs.
* * * * * * * *
the course of the traumatic event Levels of Amputation Transfemoral Amputation Upper Limb Forequarter Shoulder Disarticulation (SD) Transhumeral (Above Elbow AE) Elbow Disarticulation (ED) Transradial (Below Elbow BE) Hand/ Wrist Disarticulation Transcarpal (Partial Hand PH) Lower Limb Hemipelvectomy Hip Disarticulation (HP) Transfemoral TF (Above Knee AKA) Knee Disarticulation (KD) Transtibial TT (Below Knee BKA) Ankle Disarticulation Symes Partial Foot PF (Chopart) Toe amputation Surgical Procedures Initially, the arterial and venous supply are ligated to prevent hemorrhage (bleeding). The muscles are transected and the bone is sawed through with an oscillating saw. Sharp and rough edges of the bone are filed down, skin and muscle flaps are then transposed over the stump. Distal stabilisation of the muscles is recommended, allowing for effective muscle contraction and reduced atrophy. This in turn allows for a greater functional use of the stump and maintains soft tissue coverage of the remnant bone. Muscles should be attached under similar tension to normal physiological conditions. myodesis: the muscles and fascia are sutered directly to the distal residual bone for better prosthetic control myoplastic: suture to opposite muscle in the residual limb to to each other and to the periosteum or to the distal end of the cut bone for weight bearing purposes Ideal Stump Skin flaps: skin should be mobile, sensation intact, no scars Muscles are divided 3 to 5 cm distal to the level of bone resection Nerves are gently pulled and cut cleanly, so that they retract well proximal to the bone level to reduce the complication of neuroma Location of Pulses Femoral Triangle Foot pulse (Medial malleolus or dorsum of the foot) Popliteal (behind the knee) Femoral (within the femoral triangle) If a leg has been amputated because of gangrene, the remaining leg is examined for a puls Special Investigations Doppler Ultrasound X-rays CT scan Angiogram (outlines blood vessels) Doppler ultrasound (occlusion of vessels) Venogram and arteriogram Radioactive dye injected into the blood Arterial Insufficiency Surgery to improve circulation Bypass grafts (autogenous graft uses a vein to bypass the obstructed area) Synthetic grafts Management Please find below links to more detailed pages on the management of amputees Pain Management Pre-Fitting Management of the Patient with a Lower Limb Amputation Post-fitting Management Prosthetic Rehab High level Rehab Clinical Guidelines: Mental Health Amputees Buerger’s Exercises [4] Stimulates collateral blood flow in the patient’s leg It is performed for 20 min. The leg is elevated until the toes go white, then lowered, then level Repeat 2-3 times to improve collateral circulation Connective Tissue Massage Dynamic Stump Exercises Balance and Gait Retraining Improve static and dynamic balance Use parallel bars, walking frame then Crutches (in that order) Therapist stands on the amputation side, using a belt around the patient’s waist to support Rest if the patient feels tired [5] Short Wave Diathermy (SWD) Through the pelvis to warm the arteries (contraindicated in patients with arterial insufficiency because the warmth leads to increased metabolism, causing a greater demand for nutrients, which are not available) Post-operative Care Maintain function in the remaining leg and stump to maintain peripheral circulation Maintain respiratory function (important with smokers and those patients under general anaesthesia) Prepare for mobility rehabilitation Stump care [6] For hygiene and skin care see handout on amputations A hip flexion contracture may develop because of elevation to reduce swelling Stump bandaging is done to ‘cone’ the stump, thereby preventing oedema, which occurs because there is no muscle pump and the stump hangs Swelling must be prevented to allow proper attachment of the prosthesis, and the prevention of pressure sores The stump sock is put on first, then the prosthesis The prosthesis must be cleaned and maintained (children who are still growing, grow out of their prostheses) Mobility Aids The choice of mobility aids depends on the level of fitness, strength, balance skills of the individual: Walking frame Axillary crutches Elbow crutches Walking stick For bilateral lower limb amputees a wheelchair is often indicated (high energy expenditure during gait with prostheses) Complications Some of the most common complications associated with amputation include; Oedema Wounds and infection Pain (phantom limb) Muscle weakness and contractures Joint Instability Autonomic dysfunction See here, for more detailed information on post-operative complications following an amputation.
Prosthetics for Individuals with Hip Disarticulation/ Hemipelvectomy Amputations - Physiopedia
Introduction This is a very extensive amputation usually performed due to malignant bone tumours. Less frequently it is performed due to severe vascular disease, osteomyelitis or trauma. Due to the type of amputation, there is no residual limb left and thus no lever to control the prosthesis during gait. Socket A total embracing socket is made by making a plaster cast of the individual’s pelvis allowing the socket to enclose the iliac crest(s)[1]. The socket can be made from different types of materials. The socket for a hindquarter amputation will also contain the abdominal and pelvic contents. There are 2 main ways of casting for the socket, using forming blocks or total contact casting Weight bearing within the socket is transferred to the ischial tuberosity and buttocks of the sound limb for hindquarter amputation, and the ischium and buttock of the amputated side for a hip disarticulation amputation. [2] [3] Suspension Total tissue contact is the method used for suspension with the upper edges of the socket grasping/locking over the iliac crests. A shoulder strap can add additional suspension[1]. Prosthetic Components Feet Different feet can be used and should be chosen based upon their weight and stability it will add to the knee joint. Dynamic response feet are commonly used. Read more about Prosthetic Feet using this link. Knees Read more about Prosthetic Knees using this link, these are the pros and cons for different prosthetic knees with a hip disarticulation amputation. Single-axis knees: For individuals with a single slow speed of walking this type of knee is a favourable choice because of its lightweight and friction control. Stance control knees: Not used Polycentric knees: Used for active individuals who are able to tolerate the increased weight. With a person with a hip disarticulation with no prosthetic hip, this knee will allow some knee flexion that will shorten the leg to help with the swing. Hydraulic knees are not often used because of the increased weight but it may be chosen to initiate hip flexion during the swing phase of gait. Microprocessor knees: Even just applying a microprocessor knee as part of the prosthesis can reduce energy expenditure during gait[4]. Hip Components/Joints[5][1] Hip Limiter This is a mechanism attached on the front of the socket that allows movement of the hip in swing phase. The limiter controls movement that can be adjusted to increase or decrease step length as the individual becomes more active. A locking mechanism can be attached if required by the individual. Endoskeletal designs: Double anterior and posterior free motion hinges that allow for hip extension by means of rubber bands, and a manual hip lock. It is relatively lightweight. Sitting is difficult due to the distal components. Energy Storing Interjoint segment The individual can release energy from the hip joint by changing the amount of pelvic thrust during toe off. This will also help to control the knee extension. Foot rise is controlled and will lead to prosthesis shortening for toe clearance during swing. With this system, the prosthesis does not have to be shortened to provide for toe clearance and will prevent gait deviations like vaulting to occur. Four-bar joint/polycentric This hip joint allows for an easier and smoother walking pattern because by shortening the length of the prosthesis it helps to clear the foot during the swing phase. It is attached on the front of the socket and is therefore not in the way when sitting. Helix 3D Prosthetic Hip is an example of a more recent polycentric hip joint. This hip leads to a more natural gait by allowing for toe clearance and smooth steps. It is paired with specific microprocessor knees. In a study where robotics were applied to the prosthetic hip joint, it resulted in more symmetry during gait[4] [6] [7] [8]
Paediatric limb deficiency - Physiopedia
Children are not little adults Though there are some areas of general overlap, the management of limb loss in children is quite different to adults. Key differentiations include: A high proportion of congential limb deficiency versus acquired amputation (~3:1) Terminology / Classification An immature skeleton Adjustment Habilitation versus rehabilitation Growth and development considerations Paediatric distinctions when undergoing amputation Congenital versus acquired loss Even with nomenclature, children and adults differ when it comes to describing limb loss. In paediatrics, the term ‘amputee’ or ‘amputation’ is replaced with limb difference or limb deficiency, as the majority of children with limb loss are born this way (ie. congenital). The proportion of congenital versus acquired limb deficiency can range between 60:40 up to 75:25. For the proportion of children that suffer an acquired loss, the primary causes are: 75% traumatic (eg. lawn mower, farm machinery, motor vehichle accidents, etc). These losses are usually unilateral; 60 % are often lower limb with a distribution of Transtibial > Transfemoral > Transradial > Ankle disarticulation. Of the remaining 25% of acquired loss, malignancy and infection rank highly. Terminology/Classification Congenital limb deficiency simply means the partial or total absence of a limb at birth. Classification/description of these deficiencies has been more challenging than simply stating transfemoral or transtibial amputation levels for example in the lower limb. A variety of limb classification systems have been used over the years, including (Frantz and O’Rahilly 1961; Henkel and Willert, 1969; McCredie 1974; and Swanson 1976). The current and accepted form of classification that has been adopted internationally since 1998 and is the ISPO classification system. This form of classification utilizes anatomical and radiological evidence for describing the limb deficiency. It states whether the deficiency occurs in a transverse or longitudinal orientation and which anatomical structures are partially or totally absent.(ADD REFERENCE +/- PICTURES) Growth and Development The management of paediatric limb deficiency requires a longitudinal outlook. This is to take into account the many development stages children go through from 0-18yrs, growth spurts and the need for education and anticipatory guidance for the family. Unlike adult prosthetic prescription, a child may undergo a vast array of prosthetic changes as they grow eg. stumpies to extension prostheses with feet, to single axis knee units, to polycentric knee units, etc. On top of the management of prosthetic alterations to match growth and cognitive development, there are the skeletal immaturity factors that need to be monitored throughout childhood (ie. Growth spurts, terminal overgrowth, limb length discrepancies, etc). Possible reasons for review through a paediatric limb deficiency service: Prosthetic provision Interim prosthetic program for assessment of prosthetic proficiency Definitive prosthetic prescription Prosthetic review (eg. addition or change in prosthetic components) Prosthetic training Initial prosthetic (interim program) Specific task (eg. upper limb deficiency) Specific componentry eg. myoelectric training Developmental training (eg. walking, running, etc) Recreational prostheses (eg. musicianship) Developmental reviews Key stages of development (eg. 0-1yr, pre schooling, growth spurts, etc) Assistive and Adaptive Devices (particularly for children with upper limb deficiencies) Psychosocial support Antenatal counseling Pre amputation counseling Issues of bullying, body image, etc. Peer support Referral for genetic counseling Pain management Orthopaedic referral / collaboration Pre amputation planning Timing of epiphysiodesis Assessment and management of terminal overgrowth Conversion amputation Asymmetric deformity progression Considerations for limb lengthening Stump care (eg. skin breakdown/wound management) Pain management Anticipatory guidance (eg. medical, prosthetic, psychosocial, recreational, etc). An Immature skeletal system As is obvious, in paediatrics we are dealing with an immature skeletal system and hence issues related to growth are of primary importance. From a simple prosthetic perspective, children require more frequent prosthetic changes. In adult populations, replacement of prostheses may occur once every three years, whereas for children it is more often every year and more frequently in the early years and during adolescent growth spurts. With the rapid changes in growth there are also biomechanical and orthopaedic challenges throughout development that need to be anticipated and managed. With congential limb deficiency, issues regarding limb reconstruction and/or limb lengthening are discussions that are required for a variety of limb deficiencies eg. Proximal Femoral Focal Deficiency; Congenital short femur, Longitudinal deficiency of the fibula. Many children may choose the path of limb reconstruction rather than an amputation (commonly known as a conversion amputation). However, should the limb reconstruction path not deliver the desired goals of the child, family and treating team, then a switch to the conversion amputation may occur later in childhood. Appropriateness and timing of conversion amputations is another area of collaboration between orthopaedic and rehabilitation teams. When considering amputations, preservation of joints remains a common objection. However due to the immaturity of the skeletal system, issues such as terminal overgrowth and the maintenance of growth centres arise. In paediatrics, it is preferable for amputations to occur through joints (disarticulations) rather than through the diaphysis. This principle may lead to less cosmetic outcomes (ie. the bulbous shape of the distal stump), however the preservation of growth centres and avoidance of terminal overgrowth issues mean a better biomechanical outcome in the future and less surgical intervention throughout childhood. In the event of amputations that do occur through the diaphysis (eg. trauma), then terminal overgrowth become issues that need to be carefully monitored through until skeletal maturity. The theory behind terminal overgrowth appears to be that the cut bone is trying to create callous (as in after a fracture). This overgrowth tapers and causes distal stump pain. Clinically, it can be identified by the tapering shape of the distal stump; a bursa can often be felt under the most distal point and if severe, the area can feel warm and appear red. An x-ray is often requested to confirm terminal overgrowth. Adjustment Congenital Limb Deficiency In the paediatric population, because the majority of children are born with limb deficiency, there is little adjustment to body image for the child. However with those that acquire an amputation (be it through a conversion amputation or traumatic amputation), the issue of adjustment does have to be addressed. Though children may not go through a period of adjustment, parents and extended family members definitely do and hence support for these family members is paramount in the early phases. Ideally, if the limb deficiency is identified in pre-natal scanning, an early referral helps the clinic team meet with the family prior to birth to help address the concerns and questions parents and extended family may have. A follow up review is also advisable as soon as practicable after birth to allow the family further opportunity to discuss concerns and queries. Congenital Limb Deficiency undergoing conversion amputation Where a planned amputation occurs (ie. Conversion amputation), then pre-amputation counseling is carried out so that the child and family can adjust to the upcoming. This is often carried out with the use of therapy dolls and play therapy to illustrate the level of amputation and the use of a prosthesis in future life. The period and inclusions of pre-amputation counseling varies for each child and family. Meeting another child and family who have gone through the same or similar process can be beneficial. It assists the child to see what life after enduring the impending surgery. Pre-amputation counseling also includes clear guidance about the various phases the child and family will go through (ie. Pre-amputation planning, surgical admission, post-operative healing, stump bandaging, pre-prosthetic casting, prosthetic fitting, prosthetic rehabilitation and where appropriate participation in recreational and leisure pursuits). Post operative, medical (pain relief), physical (desensitization, contracture prevention, early mobilization, etc) and psychosocial support are utilized to continue to address the issues around adjustment. Traumatic Amputation In the event of traumatic amputations there is often no time to for counseling pre-operatively. The key factors that assist in adjustment often include timely support and again guidance as to the various phases that follow surgery. In the post-operative phase, a team approach is adopted to address pain from the surgery, phantom sensation and phantom pain. In children phantom pain is not usually a long standing issue, however in the traumatic cases (and long standing tumours), anecdotally, there is a higher likelihood of phantom pain. In traumatic cases, a greater emphasis post operatively on medical (pain relief), physical (desensitization, contracture prevention, early mobilization, etc) and psychosocial support is needed to aid in adjustment due to the absence of minimal input that can be given in the pre-amputation phase. With children and families, many childhood milestones, will cause a recurrence of grief and adjustment. Anticipatory guidance is important as a child enters child-care, the first year of schooling, sporting and recreational pursuits, etc. The focus on family adjustment is key as the child often reflects their adjustment to their limb deficiency from those that are significant in their lives (parents, grandparents, older siblings). ‘Habilitation’ versus Rehabilitation Prosthetic rehabilitation in children is often more aptly described as ‘habilitation’ as many of the skills taught are newly acquired rather than needing to be reacquired as in adult rehabilitation. Decision making around prosthetic prescription and rehabilitation are often guided by a combination of factors. Initial prescription may revolve around physical development (eg. ‘fit to sit’ for upper limb deficiencies; ‘pull to stand’ for lower limb deficiencies), but the component and rehabilitation approach often are influenced by cognitive development. For children receiving their first limb, the prosthesis is seen as a tool that can assist in play (eg. for being able to stand and cruise, reach toys that are higher, etc). It is often recommended to the family that the limb remain in the toy box when not in use, so that the child develops positive associations with the limb. For children who have a lower limb deficiency, after progressing through the developmental sequences prior to upright mobility, the issue with prosthetic rehabilitation is often that children ‘get up an go’ and hence this period of input requires adequate understanding of developmental progressions without immediately seeking a mature gait pattern. As children mature, refinement of gait can be made, but therapy is again tailored to their level of development. The primary role of paediatric prosthetic rehabilitation is not so much rehabilitation but anticipatory guidance to assist the child and family problem solve upcoming developmental milestones eg. growth spurts, commencement of schooling, engagement in sports and recreation, etc. Paediatric distinction when undergoing amputation Preoperative Phase As indicated in the ‘Adjustment’ section, where possible (planned amputations) children and families require a developmentally appropriate approach to preoperative counseling. It involves not only the child, but also parents siblings, grandparents and other significant members of the family unit. All members of the team are often involved in this phase Medical (appropriate information and guidance, pain management, etc) Social Worker (preamputation counseling) Occupational Therapist (preamuputation counseling, play therapy, home modification and/or equipment planning). Physiotherapist (preamputation counseling, physical preparation, equipment planning, guidance through the various phases to follow) Pain management involves the pre-surgical commencement of medications that may limit post-operative phantom limb pain eg. Gabapentin. Surgical Principles As indicated in the ‘Immature Skeletal System’ section, the principles that guide amputation levels are different to the adult population: Preserving growth centres is a key principle that both limits the discrepancy between limbs and allows for greatest mechanical advantage as the child grows. Preservation of joints is a key principle, much like in adults, however in paediatrics it is taken one step further, in that operations such as a rotationplasty have been developed where ankle joints can substitute as knee joints. Where the joint cannot be saved, amputations are preferable through joints rather than through the diaphysis. The primary reasons for this surgical principle is that it preserves growth centres and prevents risks of terminal bony overgrowth. In adult populations amputations through the diaphysis are preferred due to their cosmetic appearance and prosthetic socket design. Post Operatively Paediatric populations rarely have the list of comorbidities of adults and hence post-operative issues around wound healing are more related to the child’s activity rather than inactivity. Children heal relatively quickly and can be out of hospital within a matter of days to a week. Faster healing also progresses them through their post operative phase sooner and it may be as soon as 10 days post-operatively when sutures are removed and shaping of the stump may commence. Unlike adult populations, where shrinker socks appear to be more readily used, these socks rarely are appropriate or available in paediatric sizes. Often due to the uniqueness of the stump because of its anatomy (ie. Congential limb deficiencies), stump bandaging is utilized in the pre-casting phase. Prosthetic Provision Prosthetic fitting can occur as early as 3 weeks following surgery if no complications are encountered and the stump has little oedema. Paediatric prosthetic design requires a high degree of adjustability, need to be lightweight and durable. Prosthetic design also reflects developmental stages eg. Child with disarticulation may go form having stumpy (socket with peg base) in early years and progression to attachment of foot and then progression to a knee joint. The size and weight of components often dictate when a component may be added rather than simply gauging when a child is cognitively ready to use a new component eg. progression from extension prosthesis to inclusion of a knee joint. Due to rapid growth, the prosthesis may include design features unlike adult populations eg. added sockets or thicknesses of sockets, more modular components to accommodate height growth; growth oriented suspension systems, etc. Complications As indicated in the ‘Immature Skeletal System’ section, the key difference in paediatrics with regard to post-operative complications is the development of terminal overgrowth. This is far more frequent in children than in adult populations. Its recurrence can be as frequent as every two years until reaching skeletal maturity. Follow Up Paediatric limb deficiency requires far greater follow up than in adult populations due to ongoing growth and development. For this reason, it is important to see children who are using prostheses at least once a year. Many children with upper limb deficiencies that don’t use prostheses, may access the clinic ever 2-3 years. Children who are undergoing growth spurts may require reviews 3-6monthly. Resources Day, H.J.B. The ISO/ISPO Classification of Congenital Limb Deficiency in Atlas of Limb Prosthetics. http://www.oandplibrary.org
Lower Limb Amputees and Low Back Pain - Physiopedia
Introduction Low back pain is a common complaint amongst the general population[1] and is considered the leading cause of disability.[2] Amongst the adult general population low back pain has a point prevalence of approximately 12%, with a one-month prevalence of 23%, a one-year prevalence of 38%, and a lifetime prevalence of approximately 40%.[3] However, the prevalence of low back pain amongst lower-limb amputees is thought to be higher than that of the general population.[1][4][5] Back pain has been reported to affect 52% to 89.6% of lower-limb amputees.[4][5] Several studies involving lower-limb amputees have identified that low back pain is often considered more bothersome than phantom or stump pain.[6][5] In a retrospective cross-sectional survey of people with lower limb amputations (n=255) 52% rated their back pain as “persistent and bothersome” whilst 25% described it as frequent, of severe intensity, causing interference with daily activities such as social, recreational, family and work activities.[7] Subsequently, it has been acknowledged that low back pain in this population significantly affects well-being and physical and psychological health.[6][3][8] Amongst the literature, it has been hypothesised that low back pain in persons with lower limb amputation is commonly attributed to somatisation or inappropriately made prostheses, inadequately formed stump and biomechanical factors such as movement and muscle asymmetries.[8][4][9] It is thought that such asymmetries and movement impairments may result in abnormal tissue loading and deformation of musculoskeletal structures leading to low back pain and disability amongst this population.[10] No Interference (%) Minimal Interference (%) Moderate Interference (%) Severe Interference (%) Daily activities 15 43 20 22 Recreational, social, family activities 21 40 16 23 Work Inc. school and house work 24 33 15 28 Figure 1. Interference Ratings of Back Pain on Activities[7] Types of Lower Limb Amputations Within the UK, various operations of lower limb amputations are performed. Factors such as how much of the limb can be saved are considered before a method is chosen. Below illustrates a table presenting various lower limb amputations performed: Figure 2. Types of Lower Limb Amputations[11] Associated Yellow Flags Yellow flags have a valid role within the subjective assessment of low back pain within amputees, often highlighting aspects of feelings, behaviours and thoughts that can affect recovery. Several examples include: Catastrophizing Fear of movement and re-injury Distressed and low in mood Reports of extreme pain disproportionate to the condition [12][13] Amongst recent literature an association between psychological factors and measures of patient function and pain severity has been identified in persons with disabilities [14]. Depression and anxiety are prevalent following lower limb amputation [15]. Individuals are faced with many psychological threats and challenges such as physical dysfunction, alterations in self-concept, pain and changes in their lifestyle [16][17]. In addition to physical rehabilitation completed, environmental and social factors are also paramount [18]. Catastrophizing ‘the tendency to focus on pain and negatively evaluate one’s ability to deal with it’ has consistently been found to be the greatest psychological factor associated with dysfunction and pain [19][20][21]. In addition, several studies' findings highlight the significance of the social environment for amputees within the first few months after discharge. It has been hypothesized that social factors prospectively predict the development of pain and physical functioning. Furthermore, patients that are discharged with social support, however, lack solicitous environments that are less likely to develop pain, reporting reduced levels of physical dysfunction.[14] It is therefore key that an individual's values and needs are understood and treated accordingly. Hypothesis Behind LBP in Lower Limb Amputees Lower limb amputation results in a loss of somato-sensensation and motor control.[22] A person's walking depends on the integration of afferent sensory stimulation and efferent motor control for movement.[22] In order to perform daily activities amputees compensate for the loss in sensorimotor function with compensations from the intact and residual limb.[22] Asymmetrical compensatory strategies have been considered a ‘normal’ adaption following amputation; however, it has been proposed that some of these asymmetries may be ‘mal-adaptive’ causing secondary musculoskeletal dysfunctions.[10] The Asymmetrical Gait Pattern There is an evolving area of research suggesting that LBP has a chronic impact on function for lower limb amputees. There is currently no definitive cause for LBP in amputees but movement asymmetries and muscular asymmetries are hypothesised to contribute to LBP. This model [10]provides a framework which highlights the potential causes for LBP in people with lower limb amputation. Figure 3. Potential LBP mechanisms in people with lower limb amputation[10] Movement Asymmetries Time-Distance Parameters Amputees find ambulation much more difficult than non-amputees because they depend on a prosthesis for bodyweight support and gait mobility[23]. Therefore, the biomechanics of an amputees gait are altered causing asymmetries. These asymmetries can alter the distribution of load which can lead to the development of back pain[24]. Various methods have been used to determine the symmetry between limbs and energy expenditure, stance and gait speed are widely accepted means of measuring gait symmetry[23]. Energy Expenditure It is well known and accepted that energy expenditure is higher in lower limb amputees than nonamputees (NA)[25]. The mechanical efficiency of gait is thought to decrease in lower limb amputees due to abnormal movement patterns associated with their gait[26]. These abnormal patterns are the result of compensatory strategies employed to adapt to the functional loss of one or more limbs[27]. The loss of a limb results in absent joints, active and passive structures and differences in lever length[10][25]. Therefore, the compensatory strategies employed to counter this loss include greater movements of the centre of mass and compensations of the remaining intact joints, ligaments and musculature[26]. Consequently, their gait is altered and it results in lower limb amputees expending more energy than NA during gait[26]. It is generally thought above knee amputees (AKA) expend more energy than below-knee amputees (BKA)[26] [10]because BKA have an intact knee mechanism, more intact musculature and with this a longer lever which are all thought to provide better function during gait which requires expending less energy than AKA[10] [25]. Below knee amputees, exhibit increased energy expenditure over NA due to the absent ankle plantar flexors[10]. Therefore, the remaining joints and limb musculature must compensate for increasing energy expenditure. The literature is generally in agreement that AKA expend more energy than BKA. A study of 89 lower limb amputees (22 AKA, 61 BKA and 6 syme) concluded the higher the amputation the more energy expended during gait (P<0.001)[25]. Waters, Perry, Antonelli et al.[28] agreed with this and concluded AKA expend more energy than BKA. However, in this study they also reported traumatic BKA had a higher rate of oxygen uptake than both vascular and traumatic AKA, possibly due to the increased gait velocity of BKA. However, Goktepe, Cakir, Yilmaz et al.[29] reported AKA to expend more energy than BKA but the difference was not significant (P=0.35-0.75) when measuring lower limb amputees energy expenditure at different walking speeds on flat and inclined surfaces. The increased effort required during gait due to compensatory strategies employed by lower limb amputees is a possible contributing factor to the development of low back pain in LLA (Figure 3). Stance The stance phase of amputees is thought to be asymmetrical between the intact and prosthetic limb due to the altered kinematics and kinetics occurring[23]. A systematic review of 89 papers revealed those with BKA and AKA had an increased stance phase on the non-amputated leg compared to the amputated leg[30]. As a result of the increased stance phase, increased loads go through the intact joint and this repetitive stress may result in increased pain and joint degeneration experienced in lower limb amputees and with that, the development of low back pain[31] [32]. Gait Speed Lower gait speeds are reported to be linked with gait asymmetries and this is linked to the incidence of low back pain[27] [10]. Gait in amputees is generally slower than non-amputees due to the altered kinematics occurring in response to the loss of one or more limb[10]. Consequently, the function of a lower limb amputee is not as efficient compared to a non-amputee and the amputee must adapt thus reducing gait velocity[10] [25][28]. Vllasolli et al.[25], as well as measuring energy efficiency, investigated gait velocity in lower limb amputees. They concluded AKA have significantly slower gait speeds compared to BKA walking at a comfortable speed (P=<0.001)[25]. Waters et al.[28] also concluded the higher the level of amputation the slower the gait velocity. It could be hypothesised that amputees modify their gait speed to keep their energy expenditure within normal limits, something Waters et al.[28] found. This could be a protective mechanism employed by amputees so they can sustain prolonged periods of exercise without becoming exhausted[28]. Beyaert et al.[33] on a study of 15 non-amputee and 17 amputee participants concluded BKA and NA have comparable walking speed and cadence. This is possibly due to the increasing technology of the prosthetics which allow for a more normal gait pattern[10]. Faster walking speeds have been shown to increase the load on the intact limb and lead to significant asymmetry[32]. Therefore, this has the possibility to lead to the development of low back pain. Figure 4. Gait Velocity of lower limb amputees[28] Joint Motion Figure 5. AKA amputee test subject[34] Lumbopelvic & Hip According to Morgenroth et al., (2010), above knee amputees (AKA) with LBP (n=9) have increased transverse plane motion compared with AKA reporting no LBP (n=8). In addition, during gait lumbar extension increased in participants with AKA (n=17) compared to a controlled group with no disabilities (n=6) [35]. This finding however is believed to possibly be affected as a result of the control group individuals mean age (32.3) lower than the experimental group (47.5). Rabuffetti et al. (2005) observed gait in AKA (n=14) compared with the opposite leg and noted limited hip extension during heel-strike of the prosthetic limb. The authors suggested the findings were as a result of the ischial-weight bearing socket in the majority of individuals included in the study, increasing their anterior pelvic tilt throughout the stance phase. Dynamic asymmetries within the lumbopelvic region may be of significance as evidence suggests the findings observed may be a likely predisposing factor to LBP in post-amputees [36][35]. Trunk It has been observed that the majority of above knee amputees side flex their trunk towards the amputated side during the stance phase of the prosthetic leg in the frontal plane[10]. This movement asymmetry is thought to be associated with weak hip stabilising muscles (hip flexors and abductors) on the amputated side[37]. Whilst this theory remains to be tested[10], according to a study by Jaegers et al.,[38] up to 30% of the hip stabilising muscles may be atrophied in comparison with the intact side in persons with above knee amputations. The amount of atrophy is thought to be closely associated with sump length[37]. Goujon-Pillet et al.[39] also investigated trunk and pelvic movement in persons with above knee amputation (n=27). Results of this study concluded that there was a greater pelvic range of motion (p=0.05) in both the frontal and sagittal planes in persons with above knee amputations when compared to the non-disabled control group (n=33). Results of this study also observed a decrease in counter rotation between the pelvis and trunk in the transverse plane in persons with above knee amputations[39]. This may be of significance as evidence suggests that patients with low back pain also lack the ability to counter rotate the pelvis and trunk[40][41]. Fig 6A-B. Three-dimensional reconstructions of an above-knee amputation with a short stump in a ventral (A) and dorsal view (B). (1, iliacus; 2, psoas major; 3, sartorius; 4, rectus femoris; 5, vastus musculature; 6, tensor fasciae latae; 7, gluteus medius; 8, gluteus maximus; 9, biceps femoris; 10, semitendinosus; 11, semimembranosus; 12, pectineus; 13, adductor longus; 14, adductor magnus; 15, gracilis; *femur.)[38] Knee Compensatory strategies in response to the loss of a limb occur at the knee joint of amputees and this alters the kinetics and kinematics[27][10]. The knee joint is important for providing stability and propulsion during the gait cycle and to prevent wear and tear of the weight bearing joints it also has a “shock absorbing” affect[33][30]. A study of 17 unilateral, BKA concluded the intact limb undergoes a significant increase in knee flexion (between 5-9°) during the loading response compared to the prosthetic limb and to the knee flexion angles of NA [33]. Knee flexion parameters during the loading phase on the prosthetic limb is reduced by 3-9° compared to the intact limb in NA[30]. AKA often have absent or negative knee flexion on the prosthetic limb during this phase due to an absent knee joint[30]. The reduced knee flexion on the prosthetic limb is possibly to prevent the knee from giving way due to reduced strength in the knee extensors and the absence of the plantarflexors[42] [30]. Furthermore, the intact knee joint undertakes significantly more work during gait than the prosthetic limb as well as significantly more loads compared to the intact limbs of NA and the prosthetic limb of amputees[33][30]. This could be a protective mechanism to protect the stump, as it is not a natural weight bearing joint, or because of muscle weakness, decreased confidence and/or balance of the amputated leg[33]. Ankle Compensatory mechanisms employed in response to the loss of a limb alter joint kinetic and kinematics at the ankle [27][43]. This is thought to affect the stance, toe off and early swing phases of the gait cycle [30]. The ankle plantar flexors are the predominant muscles active during the toe off phase of gait and are responsible for 80% of the force produced during this phase of the gait cycle[10]. Consequently, this toe off force decreases in lower limb amputees and the prosthetic limb does around 20% of total work done by NA ankles[43]. This significantly reduces the mechanical work generated by the lower extremity during gait[43]. Due to absence of the plantar flexors, less ankle range of motion has been documented in the prosthetic limb of lower limb amputees compared to the ankle of an intact limb during stance phase of gait[27][30]. A study of 18 participants reported an increased range of motion during gait in the intact limb (26°) of amputees compared to NA (21°)[27]. However, this difference was not significant. The increased range of motion present in the intact limb of amputees is to allow them to clear the prosthetic limb during the swing phase of gait due to the limited ankle range in the prosthetic limb[27]. A study of 24 participants concluded the absence of the plantar flexors affects the ankle kinematics causing compensations[43]. Compensations include the intact limb undergoing a third more work than the prosthetic limb at the ankle joint due to the decreased push off of the prosthetic limb. Therefore, the altered kinematics and kinetics in the ankle joint could be a cause of the development of low back pain. Muscular Morphological Asymmetries Morphological changes are thought to occur in amputees due to a combination of bed rest, changes to gait compensations and inability to fully contact the distal muscles of the residual limb [44]. The composition and circumference of soft tissue around the residual limb could influence the control of prosthesis through the socket fit, comfort and ability to fully weight-bare in the prosthesis[44]. Above Knee Amputation (AKA) Following AKA, hip muscles of the amputated side can atrophy up to 30%[37]. There is a positive relationship between proximal level of amputation and degree of atrophy [37]. In 5 AKA participants, dual-energy x-ray absorptiometry identified significant muscle atrophy in residual limb (P<0.001) compared to contralateral limb this also corresponded with significant increase in percentage of fat (P<0.05). The relative limb difference of muscle cross sectional area was 117.6%±22.2% compared to the in-tact thigh[44]. Below Knee Amputation (BKA) There are significant changes in muscle and fat composition between in-tact and amputate limbs. An average of 39% difference between-limbs in fat cross-sectional area (P<0.05) and the relative difference of muscle cross sectional area between limbs was significantly less in the residual limb 104.4%±32.6% (P<0.01)[44]. Similar findings identified 17 amputees wearing patella bearing prosthetic had significant atrophy of the thigh on the amputated side (P<0.001) when compared to the contralateral limb[45] Participants underwent muscle ultrasonography and the rectus femoris, vastus lateralis, vastis medius and vastus intermedius had significant atrophy (P<0.001) but the sartorius, gracilis and semitendinosus did not. The general cross-sectional area of the thigh had reduced from ranges 69.6%–96.7%)[45]. It has been recognised in two studies that muscle atrophy in the rectus femoris of the in-tact side can occur[45]. We could hypothesise that the amputee patients may have spent a large amount of time in a wheelchair or off their feet in the initial stages of rehabilitation leading to atrophy occurring. Figure 7. Percentage of muscle thickness and cross-sectional areas on the amputated thigh compared to the contralateral muscles (ND Not determined, NS Not significant).[45] Muscle Recruitment Asymmetries Trunk AKA have significantly increased back extensor strength compared to BKA (P<0.05)[8]. This may be a compensation strategy for the lack of hamstrings and quadriceps by using their back extensors during walking. An increase in back extensor strength causes changes to neutral posture and spinal stability. In contrast, AKA have significantly reduced endurance of the back extensors compared to BKA (P<0.05)[8]. Reduced endurance may cause LBP in two ways. Firstly, when muscles fatigue additional pressure is placed on supporting structures of the spine leading to LPB. Secondly, a shorter stride length with prosthetic leg places less demands on the back extensor muscles therefore activation is reduced and instability can occur [7]. Only one study study has explored back extensor strength and LBP. This study lacks inter-rater reliability of the manual muscle strength testing and has a low statistical power (<60%). Due to a lack in research this is no comparable studies for trunk strength and LBP in lower limb amputees[8]. Figure 8. Independant t-tests for all variables grouped by amputation level.[8] Hip A systematic review of 13 articles identified major asymmetries performed in the amputated and in-tact legs during walking [22]. Both legs had increased work of the hip extensors during early stance compared to control subjects. This increase in gluteus maximus activation during walking is thought to transfer energy into the trunk to facilitate forward progression. One of the studies which support this finding identified a 270% increase in work of hip extensors during initial stance of the intact limb[27]. Both studies suggest this increase in hip extension during initial stance is thought to facilitate push off from the prosthetic limb. The prosthetic ankle only achieves 20% of the work done by a control ankle due to its reduced mobility and lack of plantarflexion[43]. Therefore this increase in hip extensor activity is a compensatory mechanism providing major source of energy for forward propulsion [43]. Similar findings in a non-randomized control study identified increased hip activity by the intact-limb[43]. Eight participants were compared against eight controls using a gait analysis system. The concentric hip extension of the in-tact limb in stance was greater than that of normal subjects and the amputee subjects (9.9+/- 5.5J vs 3.6 +/- 2.6 J). The intact-limb also exhibits a significant increase in hip flexor activity during push-off phase (p<0.05)[43]. This is considered to encourage weight transference on to prosthetic limb. Most of the asymmetries highlighted in the systematic review can be attributed towards reduced weight acceptance on to the prosthetic leg and the loss of ankle plantarflexors[22]. Knee BKA Amputees have significantly reduced strength of quadriceps and hamstrings of the affected limb (P<0.01)[46]. Isakov et al (1996) measured strength in 18 amputees using a dynamometer and observed a range of 35-60% difference in strength compared to the intact side[46]. This suggests that the in-tact leg takes a greater work load to overcome this loss in strength and facilitate walking. These findings correspond with multiple authors who identified that ground reaction force of in-tact limp during walking is greater than the prosthetic leg[33][47]. The increase in ground reaction force suggests the strength discrepancy between limbs causes amputees to rely heavily on their intact limb causing asymmetrical limb loading. The amputee relies upon quadriceps and hamstrings for forward propulsion due to the absence of plantar-flexor muscles on the prosthetic side[47]. Therefore, reduced quadriceps and hamstring strength over the amputated knee will impair the ability of the residual limb to produce enough propulsion for walking[47]. This significant strength asymmetry between knee muscles corresponds to asymmetrical movement identified by digital gait analysis[47]. Digital gait analysis identified 66% more asymmetries in the amputee group than control (P>0.05) and these findings identified correlations between strength and gait asymmetry[47]. One explanation for reduced strength in residual limb hamstrings and quadriceps is that forces on the residual limb created by walking create increased blisters, sore and discomfort on the limb which can lead to gait asymmetries, for example; extending the hip and knee reduces pressure in the socket which may lead to decreased demand on the muscles and reduced strength[47]. Lower Limb Prosthetics The prescription of a prosthetic limb corresponds to the patient’s needs and functional level. Prosthetic components have a large variance in costs therefore practitioners are require to create objective criteria for prosthetic prescription[30]. Blachfords Prosthetics and Orthotics is a worldwide leading prosthetics company which supply over 35% of the prosthetics in the NHS. The components they prescribe are based upon a graded impact and activity guide. It has been identified that different prosthetic components influence gait symmetry[48]. Participants reported they felt more confident in a certain prosthetic foot which reduced their compensation strategies. Although it may be assumed a more mobile component would create symmetry of the intact leg, it does not necessarily create a symmetrical gait. If a person does not have the energy and control to stabilise a mobile component they are likely to fatigue early causing asymmetrical movements and potentially lead to musculoskeletal disorders. Appropriate fitting of a socket improves control over the prosthesis, potentially improving proprioception and force transfer in to the residual limb[48]. This highlights the importance of MDT working to obtain maximal fit of the socket throughout their rehabilitation and amputee life. Integrated within this is the importance of teaching the amputee how to donn and doff the socket independently for maximal control over the prosthesis. There are limitations and benefits to different types of prosthetic components, for example; A trans- femoral ischium socket restricts natural hip extension and can cause compensatory mechanisms at the pelvis. A less mobile prosthetic ankle has substantial reduction in dorsiflexion potentially leading compensatory mechanism such as, hip hiking to facilitate floor clearance and over-activity in the in-tact hip [43][49][50]. Figure 9. Types of